Malnutrition deaths among Indian
children aged under five have dropped by two-thirds between 1990 and
2017, but it still remains the underlying risk factor for 68 per cent of
child deaths, according to a study published in The Lancet Child and
Adolescent Health on September 18.
The first comprehensive estimates of disease burden due to child and
maternal malnutrition and the trends of its indicators in every state
from 1990 have been published by the India State-Level Disease Burden
Initiative.
The findings show malnutrition is still the leading risk factor for
disease burden in persons of all ages considered together contributing
17 per cent of the total DALYs (disability adjusted life years).
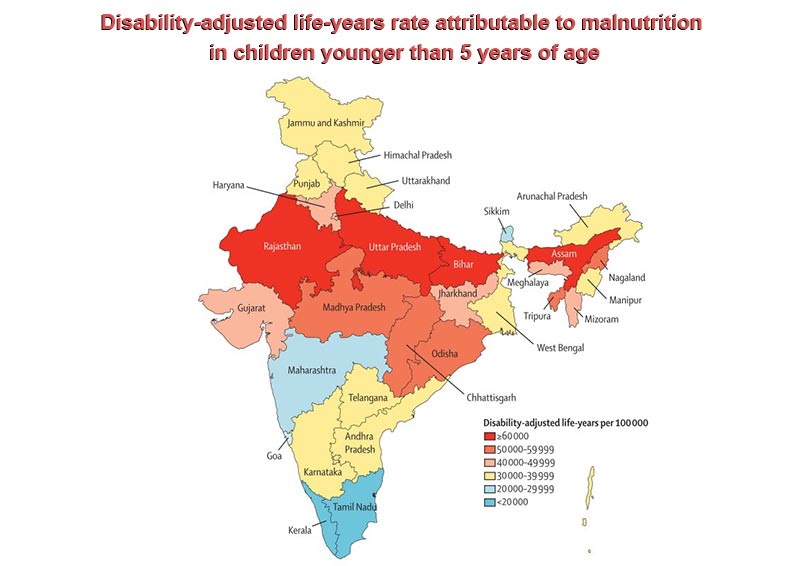
The DALY rate attributable to malnutrition in children varies
seven-fold between the states and is highest in Rajasthan, Uttar
Pradesh, Bihar and Assam, followed by Madhya Pradesh, Chhattisgarh,
Odisha, Nagaland and Tripura, the study noted.
Among the malnutrition indicators, low birth weight is the largest
contributor to child deaths in India, followed by child growth failure,
which includes stunting, underweight and wasting, the study stated.
Low birthweight a serious issue
According to the study, the prevalence of low birth weight was 21 per
cent in India in 2017, ranging from 9 per cent in Mizoram to 24 per
cent in Uttar Pradesh.
Low birthweight was the largest contributor to child malnutrition
DALYs in India, its slow decline should be addressed as a priority, the
report said.
South Asia, with India as its largest component, is estimated to have
the highest prevalence of low birthweight for any region in the world.
A major issue with tracking low birthweight is the poor quality of
birthweight data in many low-income and middle-income countries,
including India.
Low birthweight adversely affects not only child health, but also increases the risk of chronic diseases later in life.
Weight at birth is an intergenerational issue dependent on an
interplay of various factors, including maternal undernutrition,
intrauterine growth, gestation at birth, birth spacing and order, and
maternal age.
The higher proportion of underweight women in the reproductive age
group in India compared with sub-Saharan Africa has been suggested to
contribute to a higher prevalence of low birthweight in India, even
though sub-Saharan Africa is poorer.
Chronic energy deficiency in women of reproductive age is a
manifestation of long-standing malnutrition reported to be common in
India, which increases the risk of preterm births and infants with low
birthweight.
Improving the nutritional status of girls in general and that of
women in the preconception period and during pregnancy and provision of
quality antenatal care, including the treatment of pregnancy
complications, would positively affect low birthweight and extend the
benefits to the next generation.
Aligned with the Global Every Newborn Action Plan, the India Newborn
Action Plan launched in 2014 aims to reduce low birthweight through
improved preconception and antenatal care, adolescent-specific health
services, nutritional counselling, and micronutrient supplementation.
Other major issues
The prevalence of child stunting was 39 per cent in India in 2017,
the study stated. This ranged from 21 per cent in Goa to 49 per cent in
Uttar Pradesh. Its annual rate of reduction was 2.6 per cent in India
between 1990 and 2017.
Stunting, an indicator of chronic undernutrition, caused by a variety
of social, environmental and economic risk factors, is unsurprisingly
highest in the less developed states.
The prevalence of child underweight was 33 per cent in India in 2017,
ranging from 16 per cent in Manipur to 42 per cent in Jharkhand. Its
annual rate of reduction was 3.2 per cent between 1990 and 2017.
According to the study, the prevalence of child anaemia was 60 per
cent in India in 2017, ranging from 21 per cent in Mizoram to 74 per
cent in Haryana.
The high burden of anaemia in children and women, with only a modest
decline since 1990, is a major public health issue in India.
Anaemia increases the risk of adverse birth outcomes and mortality
during and after child birth and leads to poor cognitive and physical
development and mortality in children. Interventions to improve the
nutrition of girls, including reduction of the prevalence of anaemia,
starting at a young age, are needed for better pregnancy-related and
early child health outcomes and for a beneficial long-term effect on
future generations.
India launched the National Iron Plus Initiative in 2013 to
comprehensively address anaemia burden across the life cycle, through
age-specific interventions with iron and folic acid supplementation and
deworming.
The findings in the report indicate that, if the trends up to 2017
continue, the National Nutrition Mission 2022 and the WHO and UNICEF
2030 targets will not be achieved in most states of India, except for
low birthweight and stunting in a few states and exclusive breastfeeding
in several.
How can India tackle malnutrition issues?
Substantial improvements across the malnutrition indicators in the
states of India would require an integrated nutrition policy to
effectively address the broader determinants of undernutrition across
the life cycle.
These improvements include providing clean drinking water, reducing
rates of open defecation, improving women’s status, enhancing
agricultural productivity and food security, promoting
nutrition-sensitive agriculture, coupled with harmonisation of efforts
across ministries and sectors, political will and good governance, and
strategic investments in a multisectoral approach.
The government launched a revamped National Nutrition Mission with a
budget to comprehensively address the challenge of persistent
undernutrition. The goal of this mission is to systematically synergise a
variety of nutrition-related activities of various government
ministries and stakeholders in order to strengthen many maternal and
child health initiatives across the life cycle. This includes the
supplementary nutrition component of Integrated Child Development
Scheme, Maternity Benefit Programme, Mid-Day Meal Scheme, dietary
diversification to improve iron and folic acid intake, engaging the
private sector in food fortification efforts, and placing emphasis on
the broader social determinants of nutrition.
This renewed focus on a multisectoral approach to address
malnutrition is encouraging, and the targets set by the mission could
motivate the states to accelerate progress. Additionally, several
ongoing initiatives under the ministry of women and child development to
reduce gender inequality and empower women can also contribute to
improvements in malnutrition.
The major ongoing sanitation improvement drive in India under the
Swachh Bharat Mission is also expected to contribute to the reduction in
malnutrition.
The India State-Level Disease Burden Initiative is a joint initiative
of the Indian Council of Medical Research, Public Health Foundation of
India and Institute for Health Metrics and Evaluation in collaboration
with the health ministry along with stakeholders associated with more
than 100 Indian institutions, involving many leading health scientists
and policymakers from India.
No comments:
Post a Comment